Title:Effect of Parecoxib on Postoperative Opioid Requirement and Pain Control
标题:帕瑞昔布对术后阿片类药物需求和疼痛控制的影响
Authors: Jun Tang, et al.
作者:Jun Tang 等
Published in: Anesthesiology, 2002
发表期刊:《麻醉学》,2002年
Objective:
The study aimed to evaluate the effectiveness of parecoxib, an intravenous COX-2 inhibitor, in reducing postoperative opioid requirements and enhancing the quality of pain control in patients undergoing surgery.
研究目的:
评估帕瑞昔布(静脉环氧合酶-2抑制剂)在减少术后阿片类药物需求量及提高疼痛控制质量方面的效果。
Methodology:
Study Design: Double-blind, placebo-controlled trial
Participants: Patients scheduled for various types of surgeries
Interventions: Patients were randomized to receive either parecoxib or a placebo.
Measurements: Postoperative opioid consumption, pain intensity scores, and adverse effects were recorded and analyzed.
方法:
研究设计:双盲、安慰剂对照试验
参与者:计划进行各种类型手术的患者
干预措施:患者被随机分配接受帕瑞昔布或安慰剂。
测量:记录并分析术后阿片类药物消耗量、疼痛强度评分及不良反应。
Key Findings:
Reduction in Opioid Use: Patients receiving parecoxib required significantly less postoperative opioids compared to the placebo group.
Improved Pain Control: The quality of pain control was better in the parecoxib group, as evidenced by lower pain intensity scores.
Safety and Tolerability: Parecoxib was well tolerated with a safety profile similar to the placebo.
主要发现:
减少阿片类药物使用:接受帕瑞昔布的患者术后所需阿片类药物显著少于安慰剂组。
疼痛控制改善:帕瑞昔布组的疼痛控制质量更好,疼痛强度评分较低。
安全性和耐受性:帕瑞昔布耐受性良好,其安全性与安慰剂相似。
Conclusion:
Parecoxib is an effective analgesic that reduces the need for opioids and improves pain management postoperatively without increasing adverse effects.
结论:
帕瑞昔布是一种有效的镇痛药,可减少术后阿片类药物的使用并改善疼痛管理,同时不增加不良反应。
相关化合物及其CAS号
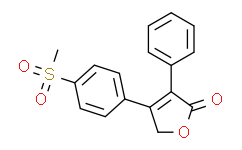
1. **Parecoxib (帕瑞昔布)**
- **CAS Number:** 198470-85-8
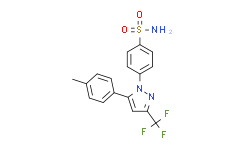
2. **Celecoxib (塞来昔布)**
- **CAS Number:** 169590-42-5
3. **Rofecoxib (罗非昔布)**
- **CAS Number:** 162011-90-7
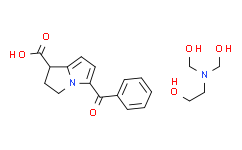
4. **Ketorolac (酮咯酸)**
- **CAS Number:** 74103-07-4





 沪公网安备31011402010657号
沪公网安备31011402010657号